What Fitness Pros Need to Know About New Blood Pressure Guidelines
By Zachary Fennel and Len Kravitz, PhD
Introduction:
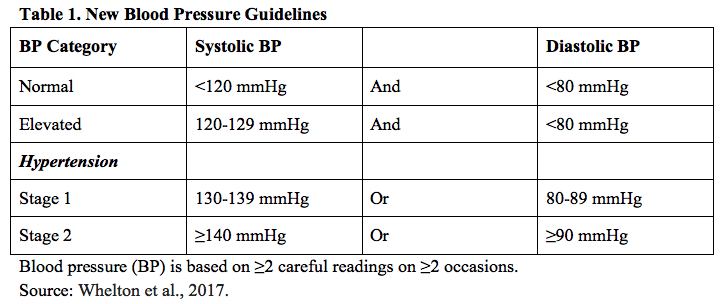
Recently, at the November 13, 2017 American Heart Association annual meeting in Anaheim, CA, the American College of Cardiology and American Heart Association released their new high blood pressure (i.e., hypertension) guidelines (See Table 1). The updated classifications now categorize hypertension stage one as resting systolic blood pressure of 130-139 mmHg or a resting diastolic blood pressure of 80-89 mmHg (Whelton et al., 2017). This updated criteria raises the previous prevalence of adults with hypertension from a reported 32% to 46% in the United States (Whelton et al.). From a health perspective, for the last 100 years scientists have observed a strong association with high blood pressure and the risk of clinical health complications (i.e., high cholesterol, kidney disease, obesity) and death from stroke and heart disease (Whelton et al., 2017). Whelton and colleagues continue that >50% of deaths from coronary heart disease and stroke occur among individuals with hypertension. The researchers explain that the rationale for the new guidelines is based from a preponderance of studies showing a high association between elevated systolic and diastolic blood pressure to cardiovascular disease. This column will review current research on high blood pressure and ways to effectively manage it with exercise and lifestyle.
|
 |
Blood Pressure and Aging
It is particularly important for personal trainers to educate clients that high blood pressure tends to increase in stages as a person ages (Whelton et al. 2017). With aging populations, there tends to be an increased incidence of 'isolated high systolic blood pressure' (Lelbach and Koller, 2017), where systolic blood pressure is elevated yet diastolic blood pressure is not. Whelton et al. add the populations developing hypertension over their lifetimes have been shown to be higher for African Americans and Hispanics as compared to whites and Asians. This gradually increasing blood pressure with age is primarily associated with structural changes in the artery walls, particularly with large arteries losing elasticity and becoming stiffer and thicker (i.e., arteriosclerosis) and the gradual development of plaque in the arteries (i.e., atherosclerosis). Lelbach and Koller submit that aging also leads to a reduced efficiency and ability of the kidneys to excrete salt, resulting in an unhealthy overload of the circulatory system, affecting both systolic and diastolic pressures.
What is the Association of Obesity to High Blood Pressure?
Lelbach and Koller (2017) highlight that in the past 20 years the risk of developing hypertension from obesity has been increasing at an alarming rate. Obesity, places a consistent strain on the heart's cardiac output (i.e., heart rate times stroke volume). Other factors associated with hypertension and obesity included disturbances with the sympathetic nervous system (which causes arteries to constrict), sodium retention, and metabolic abnormalities such as glucose intolerance (a precursor to pre-diabetes and type 2 diabetes) (Lelbach and Koller).
What is the Effect of Exercise on Blood Pressure?
Whelton et al. (2017) highlight that epidemiological studies have shown that increasing levels of physical activity and fitness result in lower levels of blood pressure and hypertension. It is meaningful for fitness professionals to share with clients that even modest levels of physical activity will help to decrease the incidence of hypertension (Whelton et al.). As well, personal trainers should educate clients that cardiovascular exercise (90-150 minutes/week; 65%-75% of heart rate reserve) and resistance training (90-150 minutes/week; 50%-80% of 1RM; multiset training with at least 6 total body exercises; 10 repetitions/set) have been shown to lower blood pressure, although the data indicate that cardiovascular exercise appears to be more effective (Lelbach and Koller, 2017). Summarizing the exercise intervention data, Whelton et al. state that on average there is an approximately 2 to 4 mmHg and 5 to 8 mm Hg decrease in adult patients with normotension and hypertension, respectively. It's important to note that individual decreases in blood pressure are variable; these numbers represent averages from studies including multiple populations and differing exercise protocols. Lelback and Koller (2017) explain that the blood pressure lowering mechanisms from cardiovascular exercise include a decrease in epinephrine and norepinephrine levels leading to a decrease of artery constriction, enhanced blood vessel function, and artery structural adaptations. All of these adaptations lead to improved blood circulation, resulting in a potential decrease in resting blood pressure.
What Dietary Strategies are Helpful in the Management of High Blood Pressure?
In the new blood pressure guidelines, Whelton et al. (2017) note the the DASH (Dietary Approaches to Stop Hypertension) diet has been shown quite effective to help reduce blood pressure. The DASH diet encourages users to reduce the sodium in their diet and consume a diet rich in fruits, vegetables, whole grains, low-fat dairy products, with reduced content of saturated and total fat. Whelton et al also note a reduction in alcohol consumption is also beneficial. The authors state that in addition to the DASH diet, it appears that low-carbohydrate and vegetarian diets have been shown to help reduced blood pressure. In regards to sodium intake, the new guidelines suggest that an optimal goal is <1500 mg/day and to aim for a at least 1000 mg/day. Figure 1 depicts other strategies that have reported varying levels of success for reducing blood pressure.
|
 |
Figure 1. Nonpharmacological Interventions that have shown to have Varying Effects on Lowering Blood Pressure.
Source: Whelton et al., 2017.
|
Final Blood Pressure Thoughts!
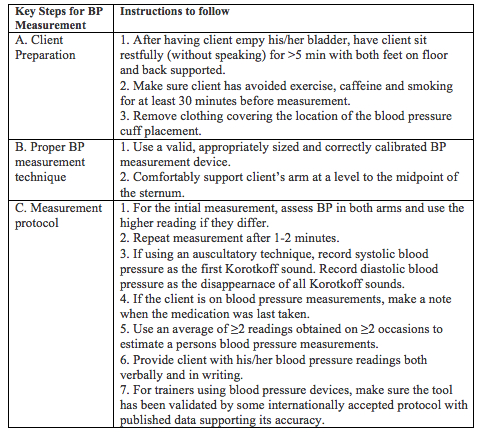
With the growing number of hypertensive individuals and the related dangers of high blood pressure, it's important for personal trainers to regularly measure middle age and over client's blood pressure (see Table 2), and to help client's develop comprehensive intervention strategies to best manage blood pressure. In the long run, a client's life may depend upon it.
Table 2: How To Measure Blood Pressure Accurately
Many personal trainers regularly assess their client's resting blood pressure. In the new 2017 blood pressure guidelines (Whelton et al., 2017), the following steps are suggested.
|
 |
Bios:
Zachary Fennel is an Exercise Science masters student at the University of New Mexico, Albuquerque. His research interests include exercise promotion, strength & conditioning, and disease prevention.
Len Kravitz, PhD, CSCS, is the program coordinator of exercise science at the University of New Mexico, where he received the Outstanding Teacher of the Year and Presidential Award of Distinction. In addition to being a 2016 inductee into the National Fitness Hall of Fame, Len was awarded the 2016 CanFitPro Specialty Presenter Award.
References:
Leibach, A. and Koller, A. (2017). Mechanisms underlying exercise-induced modulation of hypertension, Journal of Hypertension Research, 3(2), 35-43.
Whelton, P.K., Carey, R.M., Anonow, W.S. et al. (2017). ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Hypertension. 2017;HYP.0000000000000065, originally published November 13, 2017.
|
|
|
|